Abstract

Introduction:
Myeloproliferative neoplasms (MPN) include essential thrombocythemia (ET), polycythemia vera (PV) and primary myelofibrosis (PMF). Pregnancy in the presence of MPN increases the risk of thrombosis, hemorrhagic events, pre-eclampsia, progression to myelofibrosis (MF) or acute myeloid leukemia (AML) leading to poor fetal outcome.
Methods:
We conducted a literature search on PubMed, Embase, Web of Science, and Clinicaltrials.gov using MeSH terms and key words for MPN, PV, and ET from date of inception to January 2021. We excluded studies reporting less than 10 patients and those not in English language.
Results:
ET studies:
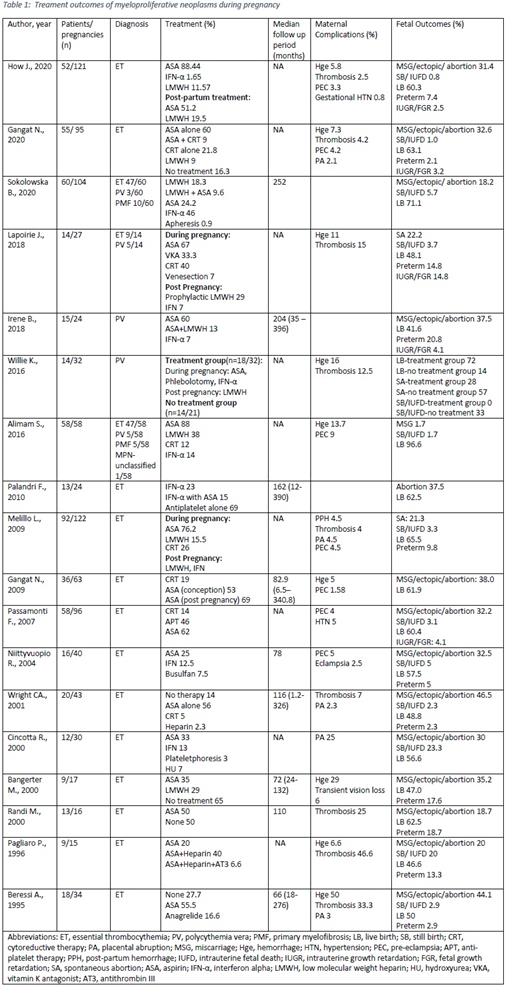
How et al. (121 pregnancy (P)/52 women (W)) reported Aspirin (ASA) was protective and was used in 51.2% P (n=62/107) with OR (odd's ratio) of 0.304 (p=0.048; 90% CI 0.102-0.795). Similar benefit of ASA was also reported by Gangat e t al.(2009) (63P/36W ; P loss 21% in 24 patients receiving ASA vs 75% in 12 patients not receiving ASA), Niittyvuopio et al. (40P/16W; live births (LB) in all 13 P treated with ASA or ASA with prior cytoreduction therapy vs 67% complications and 56% loss of P in patients not treated with ASA), Randi et al. (1999) (16P/13W; 7/13 LB occurred on ASA, and only one P was lost on ASA), Bangerter et al.( 17P/9W; 100% P treated with ASA resulted in LB vs 45% LB in P without any treatment, p=0.04), and Pagliaro et al. (15P/9W; ASA monotherapy (n=3/15P) or ASA+ subcutaneous heparin (n=7/15P) resulted in nine LB). Cincotta e t al. (30P/12W) reported 79% LB with ASA or IFN-α vs 38% LB without any treatment (p=0.06). Among the treatment cohort, 5/7 patients on ASA had a LB, and all 4/4 patients on IFN-α had a LB.
However, Beressi et al. (31P/18W) reported 4/8 untreated and 10/19 ASA treated P were lost with no statistically significant benefit. Palandri et al. reported 24P/13W treated with IFN-α (n=1), IFN-α + ASA (n=2) and ASA alone (n=9). The LB rate was not influenced significantly with treatment at conception (treated vs. untreated: 8/12 vs. 7/12, P=0.99). Melillo e t al. (122P/92W) reported no benefit with ASA. IFN-α had positive outcomes with 95% LB than patients not receiving IFN-α with 71.6% LB (OR 0.10 (95%CI: 0.013-0.846, p=0.034)). JAK2 mutation was associated with poorer outcomes (OR 6.19; 95%CI: 1.17-32.61; p=0.038). Wright et al. (43P/20W) reported no statistically significant difference between no treatment (n=16/43), ASA alone (n=24/43), ASA+cytoreduction (n=2/43), and low molecular weight heparin (LMWH) (n=1/43) groups.
Passamonti et al.( 96P/58W ) reported statistically significant worse outcomes in JAK2 negative patients, no statistically significant benefit in JAK2 positive patients (p=0.05) with ASA and higher complications with conception while on cytoreduction therapy (n=6/13 abortion, n=3/13 pre-eclampsia).
ET + Other MPN studies:
Gangat et al. (2020) reported (152W ET and 36W PV) that in 95P/55W with ET, 60% pregnancy loss occurred without ASA vs 27% with ASA (p=0.02). All 4/36W with PV who were treated with one or more of ASA, enoxaparin, and hydroxyurea delivered LB, and 50% developed venous thromboembolism. Sokolowska et al. reported 104P/60W with MPN (47 ET, 3 PV, and 10 PMF) treated with various combinations of cytoreduction therapy (IFN-α in 48P, apheresis in 1P and anticoagulation (LMWH+ASA in 10, LMWH alone in 19 and ASA alone in 24P) during the pregnancy with 72.1% LB. Lapoirie et al. stratified 27P/14W (ET 19P/9W, PV 8P/5W) with MPN into high risk (67%) and standard risk and found significant P loss in all high-risk P that did not receive ASA (n=2). Maternal complications occurred in 3 high-risk P that received ASA. 77% of P treated with ASA, LMWH, or both resulted in a LB. Alimam et al. (58W; ET 47, PV 5, PMF 5, MPN-unclassified 1) reported better than predicted outcomes in 88% of women receiving ASA during P, 38% receiving ASA + prophylactic LMWH and 3% receiving ASA + therapeutic LMWH resulting in 58 LB with a P loss rate of 1.7/100 (95% CI; 0.04-9.24).
PV studies:
Irene et al. (24P/15W) reported a 40% incidence of P loss without antithrombotic therapy vs 10.5 % P loss receiving ASA, LMWH, or both. Willie e t al. divided 32P/14W with PV into two groups (treatment group: 18 P, treated with ASA during P and LMWH for six weeks postpartum; non-treatment group: 14 P) with 72% vs 14% LB respectively.
Conclusion:
Use of ASA, LMWH and cytoreductive therapy is the existing practice for pregnancies with MPN. However, proper evidence via a RCT is an unmet need.
Anwer: Janssen pharmaceutical: Honoraria, Research Funding; BMS / Celgene: Honoraria, Research Funding; Allogene Therapeutics: Research Funding; GlaxoSmithKline: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal